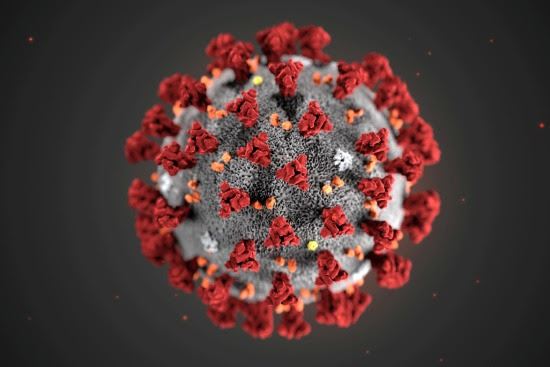
Finally, a Covid-19 vaccine developed by Oxford University’s Jenner Institute and licensed to the multinational pharmaceutical company, AstraZeneca has emerged as the favourite of World Health Organization scientists out of about 23 vaccines in their Phase III trial, after reporting success and safety in the first two phases.
For India, this vaccine is important as AstraZeneca, among others, had entered a deal with Pune-based Serum Institute of India to supply one billion doses for low-and-middle-Income countries, with first 400 million to be produced before the end of 2020. Its other global facilities will produce 300 million doses for the US.
Between April 23-May 21, Oxford University with AstraZeneca conducted human trials of the vaccine – where 1,077 volunteers were given the AZD1222 shot and all of them developed protective neutralizing antibodies as well as T-cells (T lymphocytes) which multiplied to attack any pathogen inside the human system. The participants were aged between 18 and 55 and split roughly 50-50 between male and female. Ninety-one percent of them were white, while roughly 5% were Asian, and fewer than 1% were Black.
While AZD1222 enters the next phase III of the clinical trials, the results published in The Lancet medical journal, show that the Covid-19 vaccine prompted no serious side effects among the people who received two doses so far, which has promted the WHO Chief Scientist Michael Ryan, the World Health Organization’s health emergencies chief to say: “We now need to move into larger scale, real-world trials, but it is good to see more data, more products moving in to this very important phase of vaccine discovery.” See the video below from 19:30 for WHO remarks on Oxford vaccine:
The next stage — Phase III — trial will be conducted in the US on 30,000 patients, besides those “in low-to-middle income countries including Brazil and South Africa which are already underway,” the university has said in a release.
Sarah Gilbert, professor of vaccinology at Oxford University, had earlier informed that 8,000 volunteers were enrolled for the Phase III trial which will assess how the vaccine works in a large number of people over the age of 18, and how well the vaccine works to prevent them from the infection. However, it will take a year to conclusively determine if the vaccine offers long-term protection or not.
“There is still much work to be done before we can confirm if our vaccine will help manage the COVID-19 pandemic… We still do not know how strong an immune response we need to provoke to effectively protect against Sars-Cov-2 infection,” said Gilbert.
Indian Serum Institute Role
Pascal Soriot, chief executive of AstraZeneca, said the company was on track to be producing doses by September. While the Oxford University will have intellectual property rights, Pune-based Serum Institute of India will emerge as a major supplier.
The data, published in the medical journal the Lancet, showed that the vaccine caused side effects such as fever, headaches, muscle aches, and injection site reactions, in about 60% of patients, which are deemed mild and not dangerous for any vaccine.
The Oxford-AstraZeneca vaccine AZD1222 has finally emerged as a relatively safe vaccine in view of similar results or data from others is still awaited from 22 other contestants who are in Phase III trial. In case its immediate rival vaccine from the Chinese biotech CanSino, the Phase 2 results showed that this vaccine works better in some people and not equally efficient among those aged 55 and older, a key target for Covid-19 vaccination.
Advantages of Oxford vaccine over Moderna vaccine
While the AZD1222 vaccine went on trials from April 30 with a 10,000-patient study in the United Kingdom, another 5,000-patient test began in Brazil in June and the current phase 3 results could become available in September, October, or November, said Astra-Zeneca.
AZD1222 has another advantage as it needs to be kept cold, but not frozen, whereas the messenger RNA vaccines work on the body’s genetic messaging system to provoke an immune response. The mRNA vaccines, developed by Moderna, the German firm BioNTech and the drug giant Pfizer, increased levels of neutralizing antibodies in patients.

AZD1222 works differently using a genetically engineered virus, called adenovirus, which was taken from chimps and modified not to replicate and sicken people. It carries a gene for one of the proteins in SARS-Cov-2 and inserts it into a recipient’s cells, which in turn, cause the patient’s cells to make that protein, which is then recognized by the immune system as foreign. This mechanism was not there in the past but has been used in experimental vaccines such as the Ebola virus and the virus that causes Middle East respiratory syndrome (MERS).
Oxford vaccine vs CanSino
The next rival CanSino, also into its Phase 3 trial, is a viral vector vaccine that uses a live but weakened human cold virus, adenovirus 5 — known as Ad5 for short — to develop immune system of the body to recognize the SARS-CoV-2 coronavirus. Its focus is on the Ad5 parts of the vaccine rather than the SARS-Cov-2 and many research groups have stopped it over concerns about preexisting immunity, which can run to 70% or higher in some populations.
CanSino Phase 2 trial essentially showed that those who had no or low-level pre-existing immunity to Ad5 developed neutralizing antibodies to SARS-CoV-2 at roughly double the rate of people who had high-level preexisting immunity, especially in people aged 55 and older. CanSino has dropped the higher dose.
Kathryn Edwards, scientific director of the Vanderbilt Vaccine Research Program in Nashville, Tenn., noted the CanSino vaccine may not be protective enough for older adults, but it might be useful in children. However, the CanSino vaccine has already received an emergency license in China for use in the military.