A fast, needle-free malaria detection tool developed by a University of Queensland-led team could help save hundreds of thousands of lives annually.
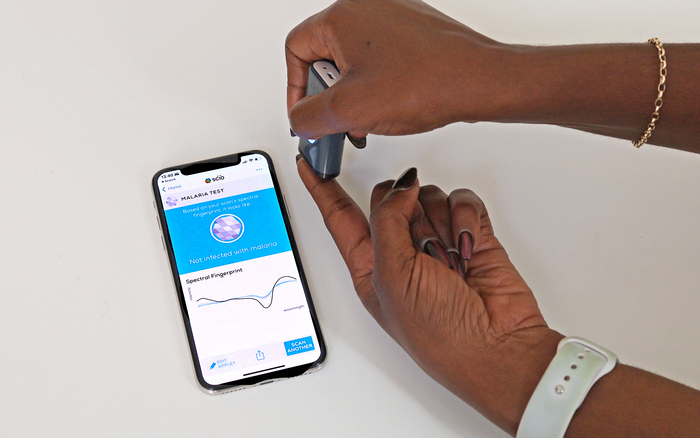
Malaria is usually detected by a blood test, but scientists have devised a method using a device that shines a beam of harmless infrared light on a person’s ear or finger for five-to-10 seconds, it collects an infrared signature that is processed by a computer algorithm.
International team leader, Dr Maggy Lord from UQ’s School of Biological Sciences, said the technology would revolutionise how malaria is fought globally.

“Currently it’s incredibly challenging to test large groups of people, such as the population of a village or town – you have to take blood from everyone and mix it with a reagent to get a result,” Dr Lord said.
“But with this tool we can find out very quickly whether a whole village or town is suffering from, or carrying, malaria.
“The technique is chemical-free, needle-free and detects malaria through the skin using infrared-light – it’s literally just a flash on a person’s skin and it’s done.
“The device is smart-phone operated, so results are acquired in real time.”
The researchers believe the technology is the first step to eliminating malaria.

“According to the World Health Organisation malaria report, in 2020 there were an estimated 241 million cases worldwide and more than 600,000 died from malaria,” Dr Lord said.
“Most of the cases are in sub-Saharan Africa, where 90 per cent of deaths are children under five years old.
“The biggest challenge in eliminating the disease is the presence of asymptomatic people in a population who act as a reservoir for transmission by mosquitos.
“The World Health Organisation has proposed large-scale surveillance in endemic areas and this non-invasive, affordable and rapid tool offers a way to achieve that.”
The technology could also help tackle other diseases.
“We’ve successfully used this technology on mosquitoes to non-invasively detect infections such as malaria, Zika and dengue,” Dr Lord said.
“In our post-COVID world, it could be used to better tackle diseases as people move around the globe.
“We hope the tool could be used at ports of entry to screen travellers, minimising the re-introduction of diseases and reducing global outbreaks.
“It’s still early days, but this proof-of-concept is exciting.”
UQ collaborated with the Instituto Oswaldo Cruz, Brazil, led by Dr Rafael Maciel de Freitas, who applied the tool to detect malaria in patients in the Amazon region.
The work was funded by Fiocruz INOVA Ideias Inovadoras, Conselho Nacional de Pesquisa e Desenvolvimento Científico e Tecnológico, Fundação Carlos Chagas Filho de Amparo a Pesquisa do Estado do Rio de Janeiro and by Advance Queensland Industry Research Fellowship and the National Health and Medical Research Council.
Also Read:
New ecology tools predict disease transmission among wildlife, humans
Japan, India scientists develop new approach to lessen severity of malaria
https://indiainternationaltimes.com/chemical-cocktail-in-skin-summons-disease-spreading-mosquitoes/6521